Medical
Nurses Are Getting Hip To Cannabis Medicine
It’s time for nurses and doctors to get trained on medical cannabis. Meet the group that’s leading the charge — United Patients Group.
Incredible medical cannabis science breakthroughs are occurring near-daily, yet the medical community remains in the dark when it comes to how just how marijuana may be effectively and safely used to treat a wide array of ailments.
Last week, The United Patients Group set out to help fix that problem by providing resources and knowledge for brave nurses willing to take on potential legal risks to provide the best medicine for their patients. At two events hosted in the San Francisco Bay Area, Alice O’Leary-Randall and Eloise Theisen — two nurses who are also incredible cannabis activists in their willingness to share their knowledge with others — lead informational workshops surrounding subjects ranging from the history of cannabis to clinical applications to treat cancer and chronic pain as well as safe dosage practices.
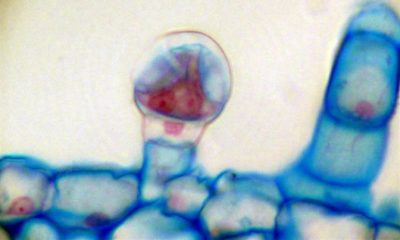
Discovered in only 1996, the endocannabinoid system and its ability to regulate homeostasis throughout the human body is still not a widely-known scientific fact. Despite centuries of patient-based stories showing benefit in marijuana’s interaction with this internal regulatory system, modern-day medicine has been unable to embrace the healing applications of cannabis due to issues surrounding its legality as well as a lack of understanding within the medical community.
“We nurses are on the front lines we have to know about this,” said O’Leary-Randall. “Legal or illegal [medical marijuana] works.”
While remaining humble in front of the roughly 30-person audience gathered for the full-day workshop on Friday at the Lafayette Library, Randall is a true pioneer in medical cannabis.
In 1976, she stood beside her late husband Robert Randall in successfully arguing for the medical necessity of marijuana before the forces of the federal government. The Randall’s decision to grow cannabis on their sunporch in Washington, D.C. and subsequent refusal to back down, in light of the pressures of a Nixon-lead government hellbent on eradicating medical marijuana, lit a fire that would change the world.
After the U.S. Government established a Compassionate Use Program that allowed Robert and a select few of other Americans to receive marijuana straight from Uncle Sam, more and more states attempted to circumvent the Controlled Substances Act with therapeutic research laws. When the AIDS epidemic of the ’80s and ’90s resulted in an increase in applications to join in the federal marijuana program, the government’s backwards response was to close the program to new applications. Spurred by this 1991 decision, states like California began a push to establish statewide medical cannabis laws and, by 2012, states across the country began to legalize cannabis for adult-use.
Randall, a retired CPN, entered nursing school after Robert passed away in 1991. She became a hospice nurse for six years before she retired in 2012 and re-emerged in the cannabis activism space.
“It was like learning a new language for me,” she said of the increasingly complicated system of cannabis laws across the U.S. that had sprung up in her short absence.
As a member of the American Cannabis Nurses Association, she now campaigns for cannabis nursing to become a recognized subspecialty by the American Nurses Association (ANA).
“The patients drive this issue,” Randall said noting that nurses, who operate in a scientific world, provide the essential bridge between the science and art present in cannabis therapeutics.
During the day-long program nurses asked questions about using cannabis for specific conditions as well as how to help their patients achieve optimal healing through application methods including vaporizing, tinctures and topicals. Theisen, an adult geriatric nurse practitioner and oncology nurse, lead presentations that included information on the way the endocannabinoid system works with external phytocannabinoids (plant-based cannabinoids) and understanding the plant’s effects through its essential oils, or terpenes.
“Stress is really what depletes our own cannabinoids,” she said, while also dispelling myths about specific cannabinoids such as CBD, which unlike THC is widely reported as containing no psychoactivity. “[CBD] does cross our blood-brain barrier and that’s the ‘high’ that people get.”
While Theisen petitioned the ANA to offer education credits for nurses participating in the class, her application went unanswered.
“But I won’t stay silent about it,” Theisen said. “It’s too important.”
Instead, nurses in attendance at these essential medical seminars of our time were offered credit through the California State Board of Pharmacy.